Infectious Diarrheal Diseases
Infectious Diarrheal Diseases
Russell Lewis
Associate Professor, Infectious Diseases
Department of Molecular Medicine
MEP 2491 Infectious Diseases
27 March 2023
Objectives
Identify the most common causes of infectious diarrhea in adult patients in resource-rich settings
Describe how the patient history and clinical presentation of diarrhea may favour viral versus bacterial causes that benefit from antibiotic therapy
Recognize warning signs for severe diarrheal disease that require immediate hospitalization and/or antibiotic therapy
Describe management approach and treatment of common infectious diarrheal pathogens
We will not be discussing (in detail) diarrheal diseases in resource-poor countries. Information on these infections should be obtained from the WHO guidelines
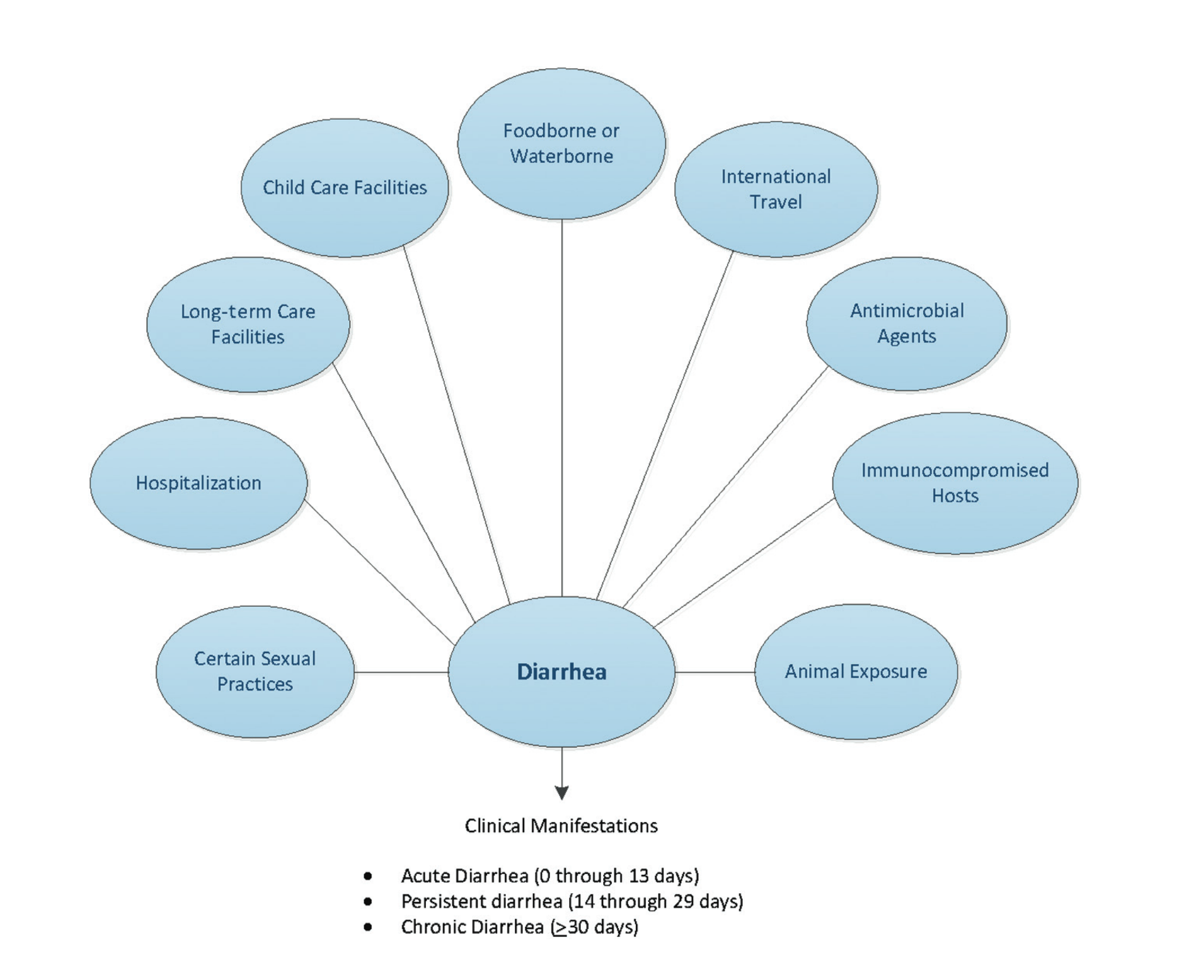
Background
- Diarrheal disease is one of the top ten leading causes of death worldwide
- Diarrheal disease is a particular concern for children younger than five years old in resource-limited settings
- Among adults in resource-rich settings, diarrhea is often a “nuisance disease” in the healthy individual
- Most cases of acute diarrhea in adults are of infectious etiology, and most cases resolve with symptomatic treatment alone
- When clinicians care for adults with diarrhea, two important decision points are:
- When to perform stool testing
- Whether to initiate empiric antimicrobial therapy
Definitions
- Diarrhea is defined as the passage of loose or watery stools, typically at least three times in a 24-hour period
- Reflects increased water content of the stool, whether due to impaired water absorption and/or active water secretion by the bowel
- Acute – 14 days or fewer in duration
- Persistent diarrhea – more than 14 but fewer than 30 days in duration
- Chronic – more than 30 days in duration
- Invasive diarrhea, dysentery- diarrhea with visible blood or mucous
- Dysentery is commonly associated with fever and abdominal pain
General Etiology
- Most cases of acute diarrhea are due to infections and are self-limited
- Most cases of acute infectious diarrhea are viral, as indicated by the observation that stool cultures are positive in only 1.5 to 5.6 % of cases
- The major causes of acute infectious diarrhea include:
- Viruses (norovirus, rotavirus, adenoviruses, astrovirus, and others)
- Bacteria (Salmonella, Campylobacter, Shigella, enterotoxigenic Escherichia coli, Clostridioides difficile, and others)
- Protozoa (Cryptosporidium, Giardia, Cyclospora, Entamoeba, and others)
Red flag symptoms- urgent investigation
- Peristent stool > 1 week
- Fever
- Bloody diarrhea
- Severe abdominal pain
- Signs and symptoms of dehydration (tachycardia, hypotension, confusion, decreased urine output)
- Weight loss
- Recent hospital stay or antibiotic exposure
- Pregnant
- Over the age of 65 years
- Diabetic, living with HIV, or immunocompromised
Norovirus “winter vomiting virus”
Norovirus
- Epidemiology
- Nonenveloped RNA virus from Caliciviradae family
- Most common cause of gastroenteritis worldwide
- Although antibody prevalence rises through childhood, re-infection is common as their is no lasting immunity due to re-infection with diversity of strains
- Transmission
- Spread by fecal-oral route from person to person, aerosol in vomitus, contaminated food and water, fomite on surfaces (resists killing by alcohol or chlorine, temperatures up to 60°C)
- Outbreaks are common
Norovirus
- Clinical manifestations:
- Vomiting
- Watery diarrhea, non-bloody and non-bilious, 4-8 stools/ 24 hours period
- Fever in 50% of cases
- Malaise, headache
- Abdominal pain
- Patients at risk of dehydration
- White blood cell count elevated or normal, lymphopenia common
- Short duration of illness (48-72 hours) with complete recovery
- Diagnosis:
- Diagnosed clinically although antigen detection (enzyme immunoassay) or PCR may be used in outbreak settings.
- Treatment:
- Supportive care (hydration)
Rotavirus
- Mean duration of symptoms for 3-8 days
- Occurs in children 6 months-2 years
- Occasionally causes diarrhea in elderly
- Vomiting less of a prominent feature vs. norovirus

Image: Centers for Disease Control
Enterotoxigenic Escherichia coli (ETEC)
- Cause of dehydrating diarrhea , especially in developing world (< 2 years age) due to ability to survive in water and production of heat-stabile and heat-labile toxins
- Causes watery diarrhea in returning travellers with nausea but no vomiting and symptoms lasting as long as 5 days
Enteropathogenic E. coli (EPEC)
- Diarrhea common in children < 6 months in developing world
- Sporadic outbreaks in adults
- Severe diarrhea that can result in dehydration and malnutrition
Entero-hemorrhagic E. coli (EHEC)
or Shiga toxin-producing E. coli (STEC)
Incubation of 1-4 days
Main serotypes E. coli O157:H7 or E. coli O101:h4 (STEC)
Often cause bloody diarrhea, abdominal tenderness with lack of fever
Occasional cause of pseudomembranous colitis (when negative for C. difficile)
Increased white blood cell count
Associated with outbreaks (contaminated food)
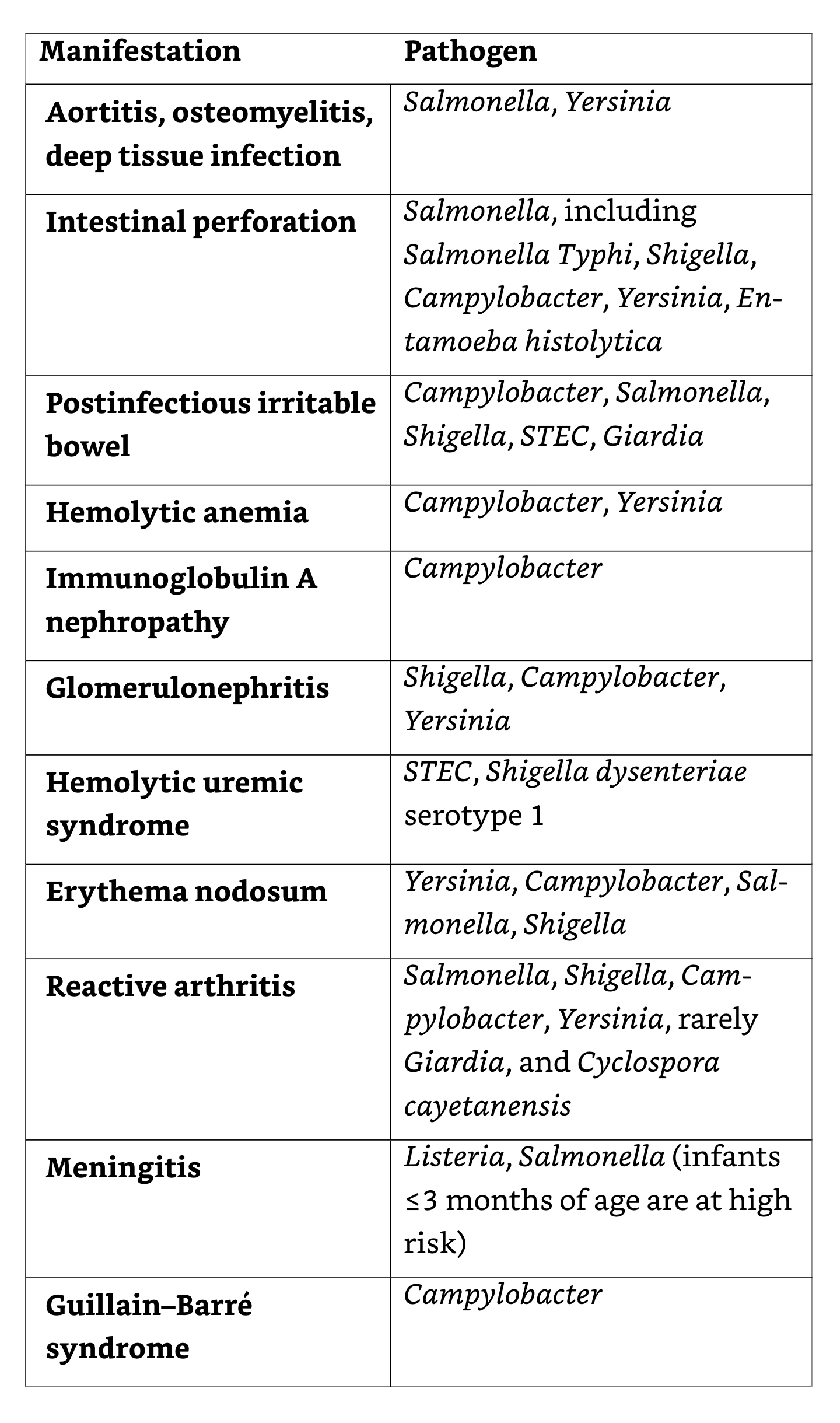
Can cause hemolytic uremia syndrome (5-10 days after diarrhea) 6-9% of EHEC infections affecting mostly children < 10 years:
Renal failure
Thrombocytopenia
Thrombotic microangiopathic anemia (↓ PLT count, haptoglobin, RBC, ↑LDH, SeCr)
Neurologic symptoms-motor deficits and seizure (4%)
Schistocytes seen in peripheral blood with
HUS
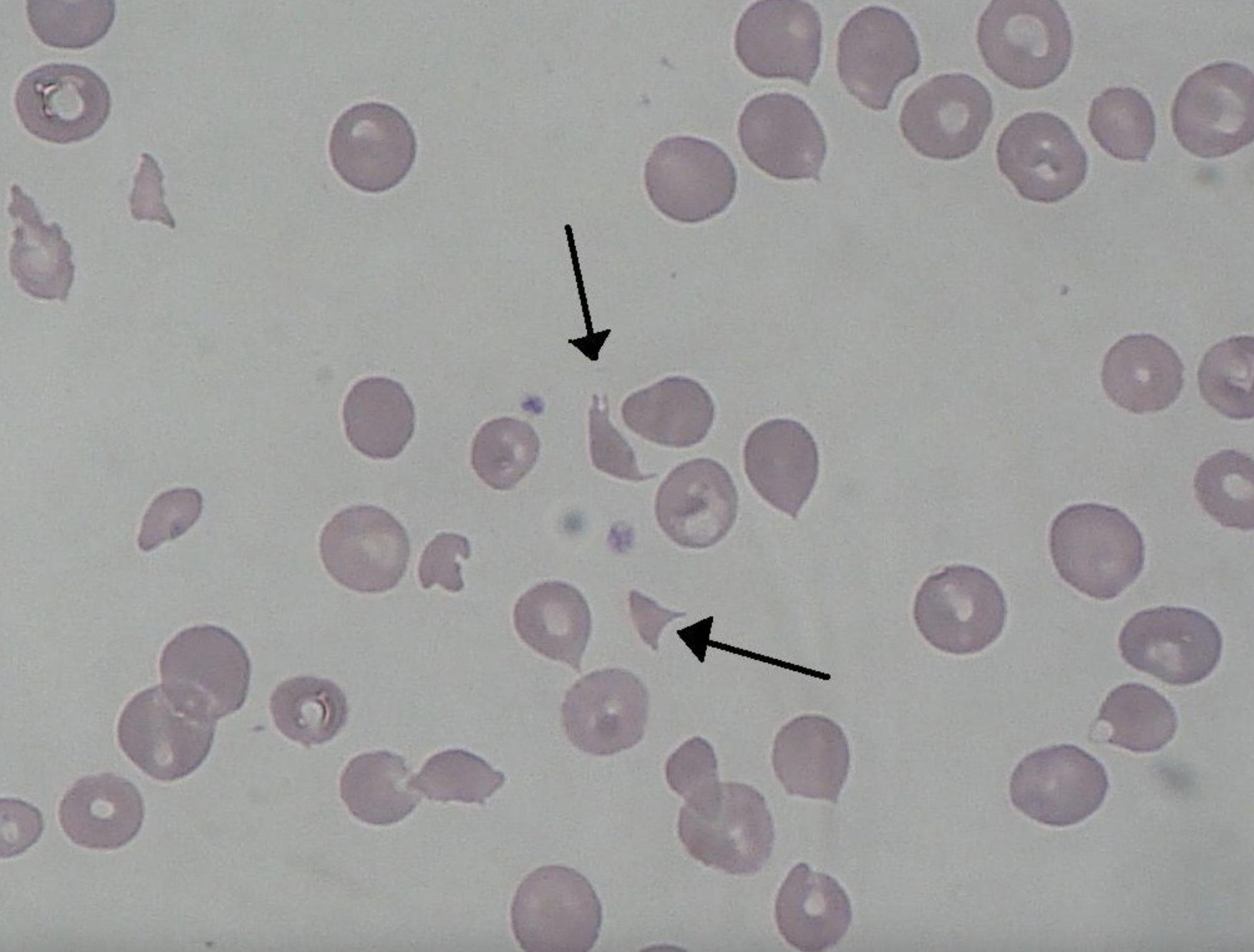
HUS long-term sequelae
- Renal failure and hypertension (39%)
Italy: E. coli 0157:H7
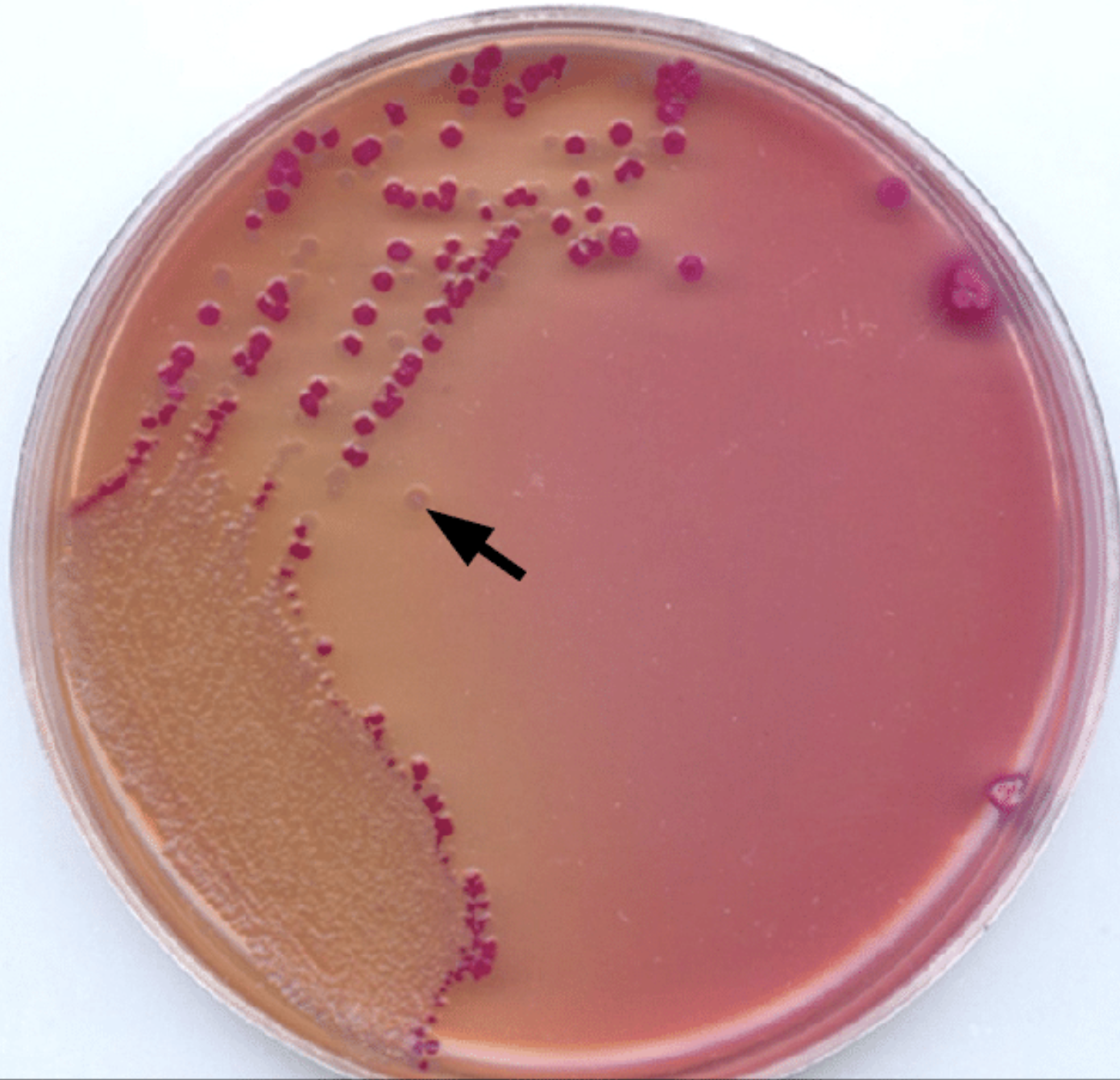
How can E. coli O157 infection be detected?
- Culture on sorbitol MacConkey (SMAC) agar with first 6 days of bloody diarrhea
- E. coli O157 cannot ferment lactose, but can ferment sorbitol
- Toxin detection (Shiga toxin, EIA in stool)
Why is it important to identify E. coli 0157 (EHEC)?
- Tracing an outbreak (i.e. contaminated produce)
- Antibiotic therapy increases the risk of HUS in EHEC by 25% and should be avoided, especially in young children
- Treatment with supportive measures and avoidance of anti-motility agents (e.g., loperamide) to reduce the risk of complications
Other E. coli- Enteroinvasive (EIEC) and Enteroaggregative (EaggEC)
- EIEC relatively rare, closely related to Shigella
- Often watery diarrhea- rarely progresses to bloody diarrhea
- EaggEC
- Affects the immunocompromised
- Cause of persistent diarrhea in patients with HIV
- Affects young children more frequently
- Can often be eradicated with antibiotics
Campylobacter
- Gram-negative that belongs to the Enterobacterales (previously known as a Vibrio-type organism associated with abortion in cattle and sheep)
- Seen worldwide and a leading cause of gastroenteritis, including in the Arctic and temperate areas
- Campylobacter jejuni most common species
Campylobacter transmission
- Common commensal in GI tract of wild and domestic animals, poultry and birds
- Food handlers: good hand hygiene essential; meat should be cooked to high temperatures (82°C, 180°F).
- Don’t drink unpasteurized milk
- Infection can occur from eating undercooked meat
- Campylobacter survive in freshwater (including at temps below (15°C) → infection from swimming or drinking contaminated water
- Direct transmission from infected animals, pets, carcasses- handwashing should be encouraged especially for vulnerable adults or children visiting farms or petting zoos
- Person-to-person transmission (nursery staff working with infected children)
- Sexual transmission
- Increased infection risk in patients with increased gastric acidity (achlorhydria or proton pump inhibitor use)
Clinical features of Campylobacter infection
- Mean incubation 3 days (range 1-7)
- Campylobacter can affect either large or small bowel, hence causes both watery and bloody diarrhea
- Classic prodrome: Fevers, rigours, dizziness in 1/3 of patients prior to GI symptoms → increased severity of disease
- Abdominal pain:
Abrupt, sever, cramping, colicky, periumbilical- not always accompanied by diarrhea
Radiates to right iliac fossa in time, mimicking appendicitis and may persist after diarrhea settles
Nausea and vomiting (15-25% of patients)
Bacteremia (0.1-1%), especially immunocompromised, hypogammaglobulinemic
Campylobacter complications
- Guillian-Barré disease
- Acute, immune-related polyneuropathy that occurs 1-2 weeks after infections
- Linked to Campylobacter infection in 3-40% of cases, alterative variate Miller-Fischer
- 100-fold higher incidence vs. population following C. jejuni infection
- Mechanism: Antibody formation that cross-reacts with GM1 ganglioside present in peripheral nerve myelin
- Reactive arthritis
- Seen in 2.6% of patients, not related to severity of illness
- Linked to HLAB27
- Onset 1-2 weeks after infection, affecting joints, wrist, knees, ankles
- May last for several weeks to months
- Typically resolves, treated with non-steroidal anti-inflammatory agents (NSAIDS)
Campylobacter diagnosis
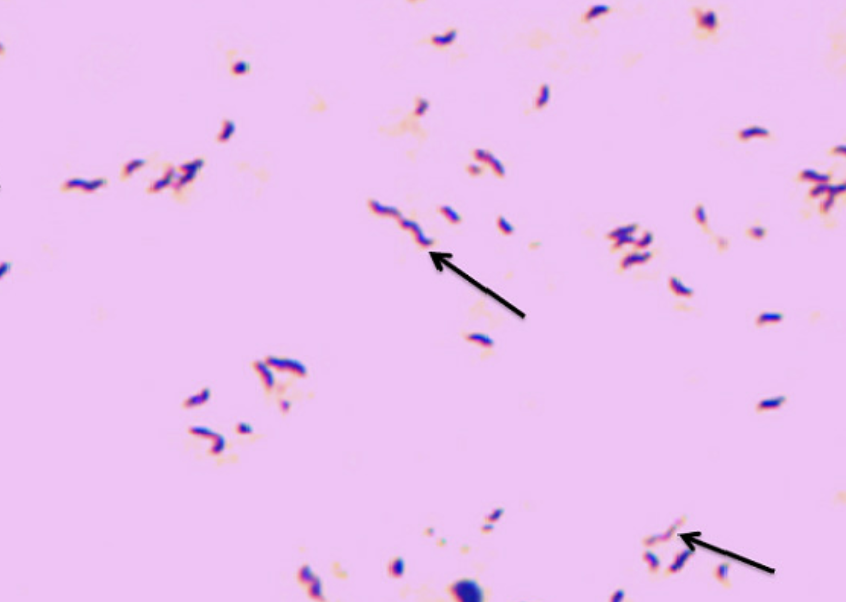
Stool culture Gram stain
Campylobacter infections: Treatment
- Generally self-limiting, antimicrobial resistance a problem (e.g., fluoroquinolone resistance in SE Asia)
- Antibiotic treatment has been shown to reduce symptoms duration by 1 day, but is indicated when patient is:
- Immunocompromised or pregnant
- Has severe disease with fever, bloody diarrhea, symptoms > 1 week, relapsing symptoms, or extraintestinal disease
- General approach: ciprofloxacin/levofloxacin or azithromycin x 3 days or until sings and symptoms have improved
- 7-14 days therapy recommended in immunocompromised
- In severe infections with bacteremia or patients unable to tolerate oral medication: carbapenem + aminoglycoside
Salmonella
- Motile Gram-negative bacteria that belong to the Enterobacterales
- Can cause:
- Gastroenteritis with non-typhoidal Salmonella spp.
- Enteric fever (Salmonella typhi and Salmonella paratyphi)
- Bacteremia and endovascular infections
- Osteomyelitis and deep-seated metastatic abscess
- Asymptomatic carriage
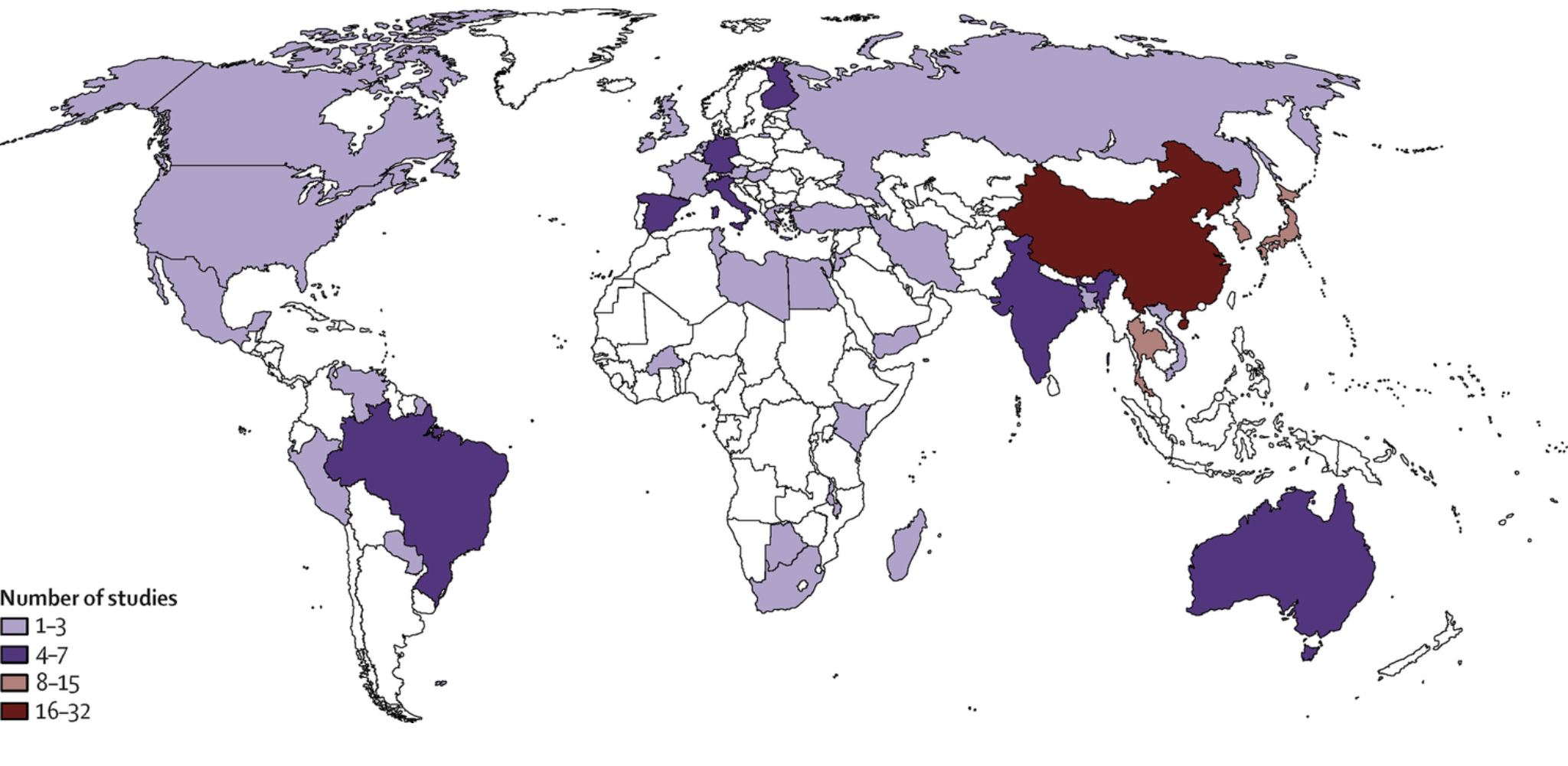
Salmonella epidemiology
- Non-typhoidal Salmonella causes inflammatory diarrhea worldwide
- Salmonella enteritidis and Salmonella typhimurium are the most common causes of diarrhea
- Highest incidence: Asia (4 per 100 cases); second to norovirus in other developed countries
- Seasonal variation with peaks of infection in summer and autumn
Salmonella transmission
- Feco-oral route; ingestion of poultry, eggs, and meat products including fresh produce
- Transovarial transmission can occur from infected henst to intreact egg shells, subsequently resulting in infection
- Contaminated infant milk
- Contact with animals colonized with Salmonella spp. (snakes, iguana, lizards, frogs, turtles in particular) also mice, rats , hamsters, cats, dogs, chickens, ducklings
- Petting farms and zoos
- Travel oversees and poor food and water hygiene
Clinical features
- Incubation period of 8-72 hours following ingestion of contained water/food (inoculum dependent
- Severity of symptoms related to bacterial dose- mild symptoms and asymptomatic carriage can occur
- Diarrhea with abdominal pain that resolves in 4-7 days, nausa, voming and fever generally resolve in < 72 hours
- Bloody stools in children
- Less than 5% of non-typhoidal Salmonella develop bactermeia
- However, when bacteremia develops: mycotic aneurysms, abscess, osteomyelitis, infective endocarditis, endovascular infection
- Patients with achlorhydria, inflammatory bowel disease, sickly cell disease are susceptible to more severe infection
Antibiotic treatment
- Guided by antimicrobial sensitivity when possible
- Preferred agents: fluoroquinolones (ciprofloxacin, levofloxacin) but resistance increasing
- Alternatives: ceftriaxone, azithromycin, trimethoprim-sulfamethoxazone
- Treatment duration:
- 3-7 days with severe GI disease but no bacteremia
- 3-14 days if at risk for endovascular infections or joint complications; or older patient
- Immunosuppressed patients have problems clearing Salmonella because it persists in reticuloendothelial cell system (RES)- prolonged treatment is required and patients are at higher risk for metastatic infections
- 14 days minimum to prevent infection relapsing or persisting
- Patients with HIV with gastroenteritis may require 2-6 weeks of therapy
Asymptomatic carriage
- Compared to other serotypes, Salmonella typhimurium is cleared quickly (less carriage)
- Following symptomatic infection, excretion can continue fora prolonged period-5 weeks
- Shedding can be intermittent, hence several cultures are required to detect carriage
- Previous short course antibiotic therapy does not reduce carriage, and may prolong shedding
- Chronic carrier states
- Continued shedding for over 1 year (0.6-2%)
- More common in women, older adults, young children, biliary tract abnormalities (e.g., gallstones)- may require cholecystectomy
- Can attempt prolonged antibiotic therapy for clearance:
- Quinolones 4-6 weeks, or amoxicillin or ampicillin 6 weeks or trimethoprim-sulfamethoxazole for 3 months
- Follow-up cultures after 6 months performed to confirm eradication
- Local health policies have specific rules about return to work (food handlers, healthcare workers)
- Continued shedding for over 1 year (0.6-2%)
Enteric fever or typhoid
(Salmonella enterica serotype typhi)
- Humans the only know reservoir for infection
- Transmission through fecal-oral route, through direct contact with infected individual or indirect contact through food or water
- Common in impoverished areas of the world
- Highest rates in South-East Asia and East Africa
- Afflicts young children and Elderly
- Often seen in returning travellers from Endemic areas- risk of antibiotic resistance
- 1-6% have chronic carriage with shedding in urine and stool for > 12 months after infection (esp. biliary tree infection with stones)
Clinical features of enteric fever-1
Stepwise over a series of weeks:
- Week 1: Fevers > 40°C with bacteremia, chills, rigours, bradycardia with pulse temperature association (see FUO lecture)
- Patients may initially present with constipation, whereas diarrhea is more common in children and patients living with HIV
- Week 2: Abdominal pain, “rose spots”
![]()
Spec et al. Comprehensive Review of Infectious Diseases - Week 1: Fevers > 40°C with bacteremia, chills, rigours, bradycardia with pulse temperature association (see FUO lecture)
Clinical features of enteric fever-2
- Week 3: Abdominal perforation secondary to necrosis and lymphatic hyperplasia of Peye’s patches (uncommon in children < 5 years), hepatosplenomegaly, intestinal bleeding and secondary bacteremia → septic shock
- Extraintestinal manifestations: headache 44-94% “typhoid encephalopathy”, altered sleep patterns, myelitis, acute psychosis, signs of upper neuron disease, ataxia, parkinsonism (but meningitis is rare)
- Bacteremia can seen cardiovascular, hepatobiliary, respiratory, genitourinary nad musculoskeletal system
- Laboratory findings: leukopenia with anemia, but leukeocytosis seen in children or with intestinal perforation
- Most patients resolve the infection in weeks to months without antibiotic therapy (cause of FUO) although death can occur with abdominal perforation
How to establish typhoid fever diagnosis?
- Blood and stool cultures (blood positive in 40-80%; stool 30-40%)
- Bone marrow > 90% recovery- considered for complicated cases or if unresponsive to treatment (will remain positive at least 5 days after antibiotic treatment)
- Serology (anti-S. typhi antibiotics ) less frequently used
Typhoid fever treatment
- Fluorquinolone and 3rd generation cephalosporin resistance increasing in SE Asia
- However, most strains still susceptible to 3rd generation cephalosporins and azithromycin, treatment of 10-14 days required
- if no resistance suscepted, ciprofloxacin, which is bactericidal and concentrates intracellularly and in the bile will results in more rapid intraceiilar clearnace than beta-lactams
- Alternatives azithromycin (5 days), ampicillin, tremimethoprim-sulfamathoxazole
- In uncomplicated cases, patients will defervesce in 4-6 days
- Relapse usually occurs after 2-3 weeks following fever resolution (depending on antibiotics) and requires further antibiotic treatment
Shigella
- Nonmotile Gram-negative facultative anaerobic bacteria belonging to Enterobacterales
- S. dysenteriae (Serogroup A)
- S. flexneri (Serogroup B)
- S. boydii (Serogroup C)
- S. sonnei (Serogroup D)
- 3rd most common cause of gastroenteritis after Salmonella and Campylobacter
- Humans are the only known host and reservoir (spread from infected food water-fecal-oral)
- Sexual transmission (anal intercourse) and epidemiologically linked to azithromycin resistance
Clinical features of Shigella infections
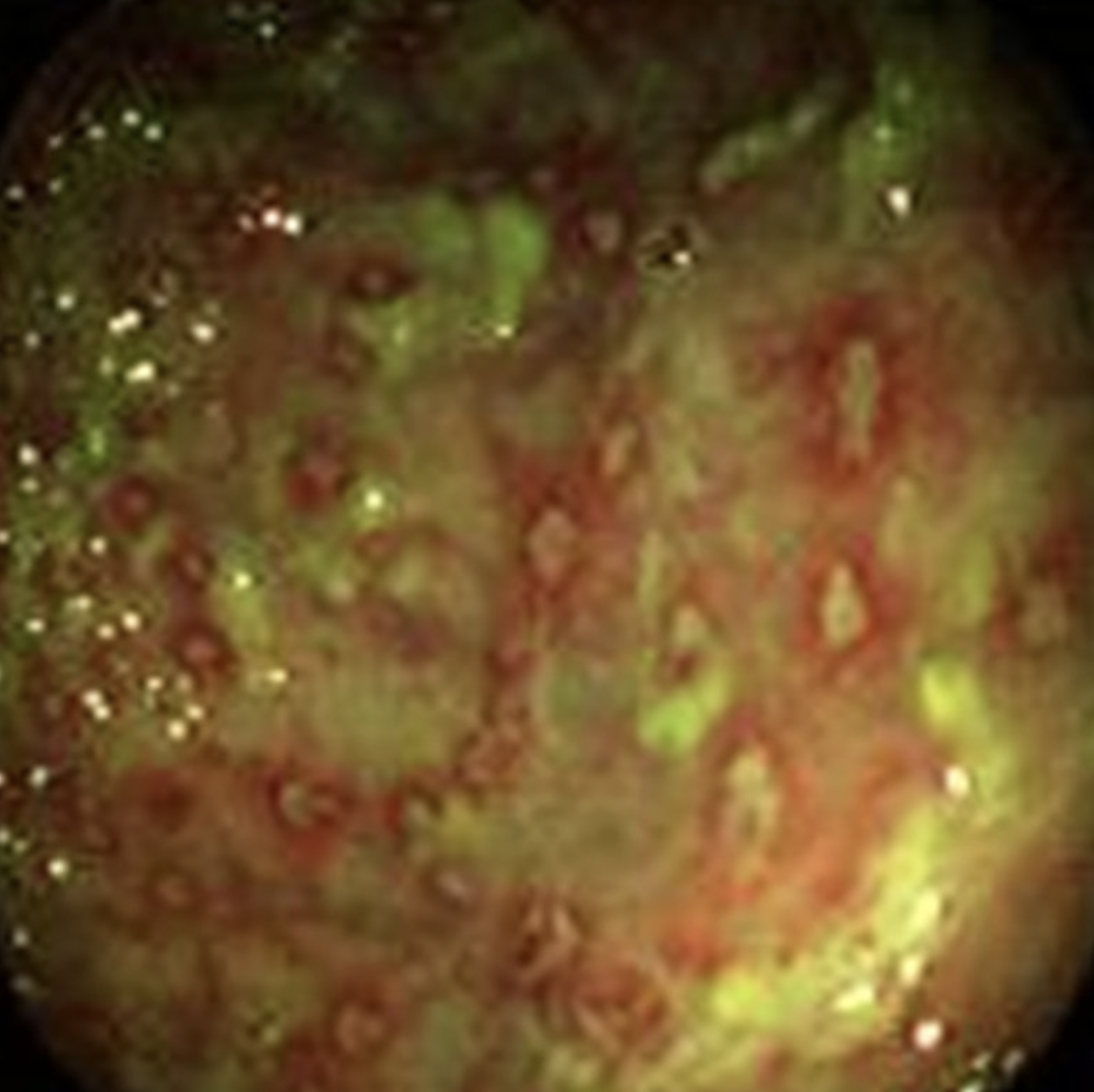
- Invade the colon mucosa cells causing abscess formation and ulceration
- Spread from cell to cell and produce enterotoxcins (plasmid-encoded ShET2), chromosomally-encoded ShET (S. flexneri) and shiga toxicn (Stx) (S. dysenteriae)
Toxins result in loss of water and solutes
Cause HUS similar to E.Coli 0157 (Stx toxin)- 8% of children
![]()
Diagnosis and treatment of Shigella infections
- Best culture yield from mucous stool
- White blood cells and red blood cells commonly seen by microbiology
- PCR testing of Shigella, but culture important for susceptibility testing
- Asia and Africa: 20-30% resistance; TMP/SMX 65-85%
- Antibiotic decrease duration of shedding and symptoms by 2 days
- Most infections are self limiting, but antibiotics are considerd for:
- Immunocompromised, including patients living with HIV
- Bacteremia or extraintestinal disease
- Patients at risk transmitting to others (Food handlers, residential home workers, nursery staff)
- Drug of choice (no resistance concerns): fluoroquinolone; or ceftriaxone pending susceptibilities
Yersina
Yersiniosis, causes by Yersinia entercolitica or Yersinia pseudotuberculosis is a zoonotic infection
Associated with unpasteurized milk, undercooked meat (especially pork), water contaminated with feces- pigs are common source of infection
After ingestion, organism proliferates in lymphoid tissue of small intestine where it may cause hyperemia, neutrophil infiltration and ulceration
Patients may present with pharyngitis (20%)- not seen with other causes of gastroenteritis
- Throat cultures may be positive
Yersina presentation
- Incubation period 1-14 days
- Localization of pain to right lower quandrant may be a diagnostic clue
- Hematogenous spread can lead to abscess infmation in the liver, spleen, mesenteric adenitis, terminal ileitis, pseudoappendicitis
- Post-infectious immunologic sequale (reactive arthritis, erythyma nodosum)
- No established data that antibiotic treatment is beneficial for uncomplicated disease, fluroquinolones may be given- IV ceftriaxone or cprofloxacin in septic patients
Vibrio
- Natural inhabitants of brackish and salt water worldwide
- Diarrhea causing species are:
- Vibrio cholerae (causative agent of cholera)
- Epidemic: V. cholerae O1 (clasical and El Tor)
- New Serogroup 0139 Bengal merged from Southern India
- Epidemic: V. cholerae O1 (clasical and El Tor)
- Vibrio parahaemalyticus
- Vibrio vulnificus (can cause diarrhea, but isolated from blood and tissues of patients with liver disease
- Vibrio
- Vibrio cholerae (causative agent of cholera)
Vibrio transmission
- feco-oral
- Cholera outbreaks are most often associated with contaminated water and contaminated food, particuliarly undercooked or raw seafood
- V. cholerae O1 and O139 are producers of cholera toxin (CT)
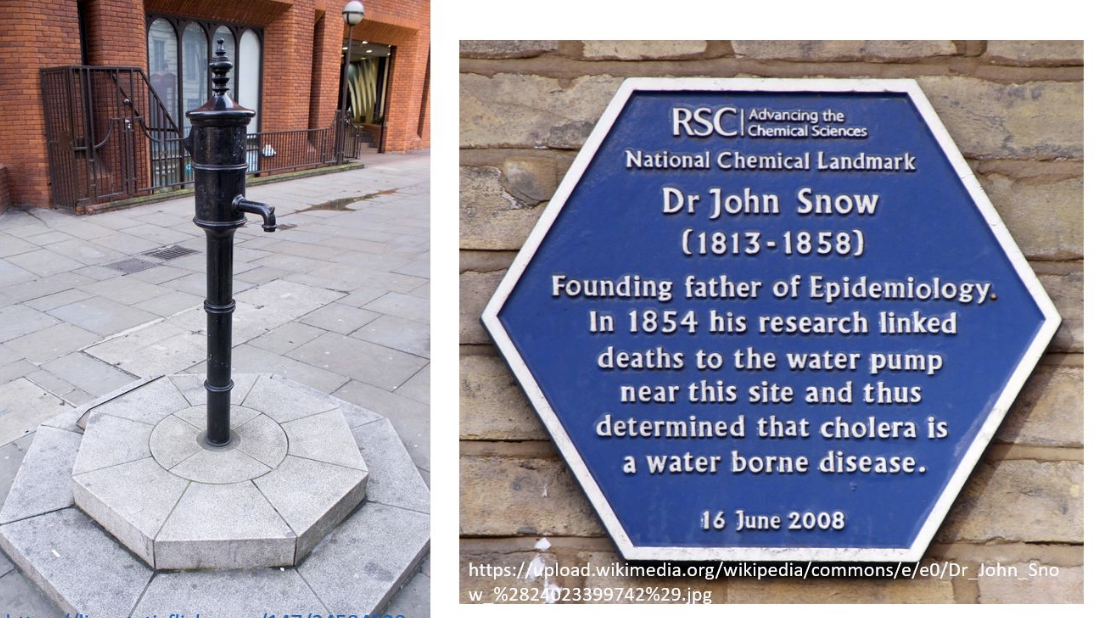
John Snow, London

Vibrio clinical features
- Profuse, watery diarrhea “rice water stool”
- Mucous, but no blood present
- Incubation: A few hours to a few days
- Significant hypovolemia and electrolyte abnormalities can occur within a few hours of symptom onset
- Abdominal discomfort, borborygmi, and vomiting are common
Vibrio treatment
- Antibiotics shorten the duration of diarrhea, reduce the volume of stool losses, and decrease the duration of V. cholera shedding
- Treatment options include macrolides, fluoroquinolones, tetracyclines based on local resistance profile
Vibrio vulficans
- Ingestion of shellfish may give rise to cellulitis and bullous lesions (especially in cirrhotic patients)
- Especially in water temperatures above 20°C (only eat raw oysters in months that end with “R”)
- Infection can progress to invasive disease with bacteremia and systemic disease in immunosuppressed, those with cirrhotic disease or hemochromatosis
- High mortality rate with septicemia- exceeds 90% if patients present with hypotension
- Patients require immediate antibiotic therapy (tetracycline + 3rd generation cephalosporin) and transfer to the ICU - Fluroquinolone monotherapy alternative

Clostridioides (formally Clostridium) difficile
- Will be discussed separate lecture in greater detail
- Gram-positive anaerobic bacillus that is spore forming and able to produce toxin
- C. difficile causes an antibiotic-associated inflammatory colitis and in the commonest cause of healthcare-associated diarrhea
- Infection requires spores to be acquired and for gut microbiota to be disrupted, usually through preceding antibiotic therapy
- Toxin A causes inflammation with intestinal fluid secretin and dmage to mucosa
- Toxin B, more potent than Toxin A, acts as a virulence factor
- Diagnosis is established with 2-step process: glutamate dehydrogenase (GDH) and PCR testing or other NAAT for toxin
- Treatment: Oral vancomycin or fidoxamine > metronidazole
Others
- Aeromonas
- Plesiomonas shigelloides
- Listeria (1% but associated with outbreaks in summer-high risk foods, unpasteurized milk
- Can cause invasive disease in pregnant and immunocompromised
- Oral amoxicillin or trimethoprim/SMX
Parasites
- Consider if diarrhea lasts > 14 days
- Giardia, Cyclospora, Cryptosporidium spp.
- May be assocaited with community waterborne outbreaks
- Diagnosed by stool culture and examination for ova, cysts and parasites
- Shed intermittently: May need 3 consecutive samples
Toxins
- Clostridium perfringes spores poorly cooked or stored meat
- Type A : cause of outbreaks- infection through poorly heated food and meat products (spores survive reheating)
- Types B and D do not produce disease
- Type C : Hemorrhagic necrosis of the jejunum (pigbel disease) following consumption of pork products. Trypsin inhibitors in sweet potatoes may inhibit breakdown of toxin and potentiates the disease
- Staphylococcus aureus toxin
- Bacillus cereus (rice) toxin
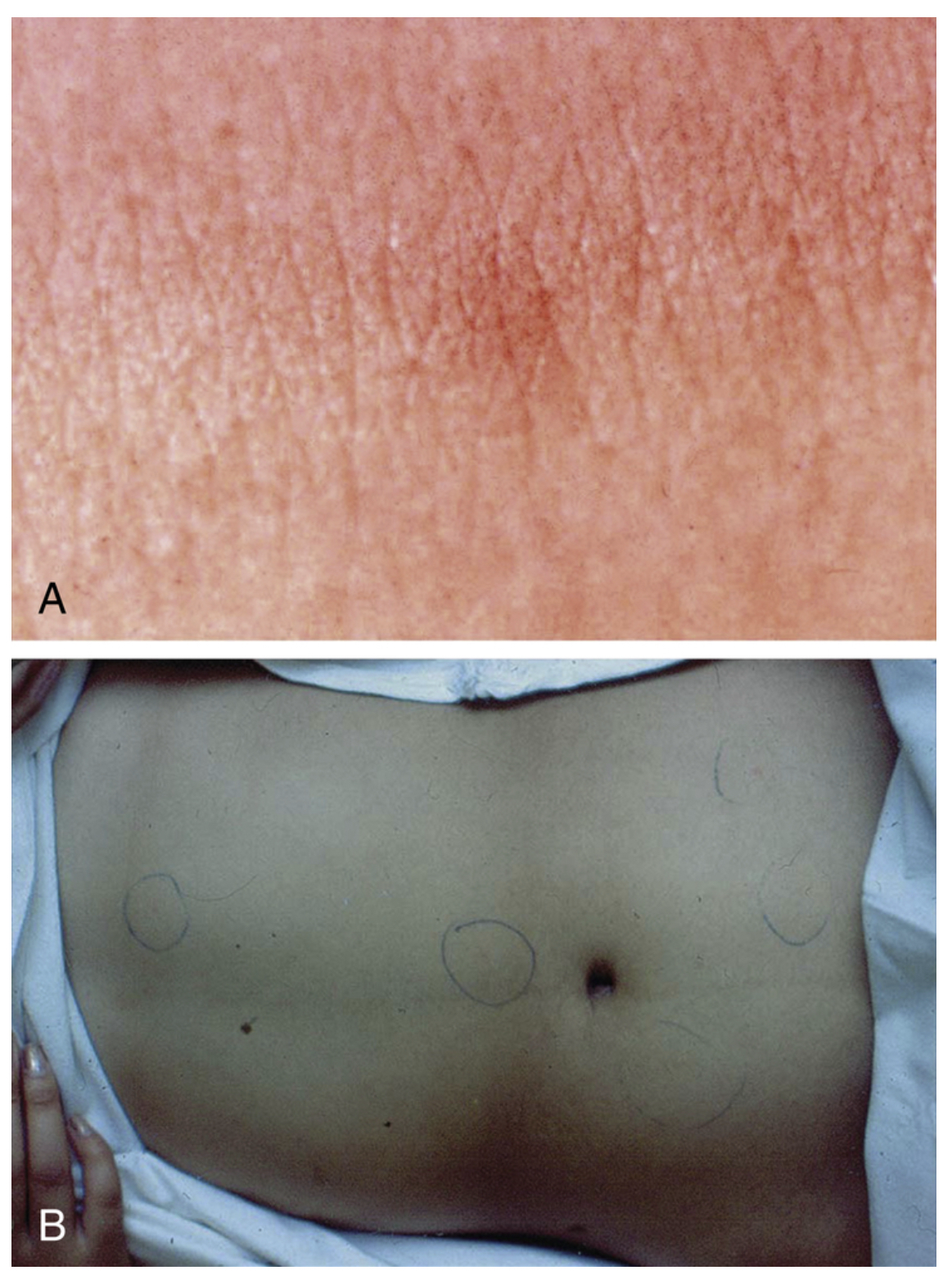
Scombroid
- Food poisoning associated with seafood
- Commonly misdiagnosed as allergy
- Incorrect storage above 4°C, resulting in bacterial overgrowth and build up of toxic levels of histamine and other biogenic amines by the bacterial enzyme histidine decarboxylase found in dark fish meat
- Scombridae and Scoberesocidae: tuna (even open cans), mackerel, skip-jack, bonito, dolphin, tilapa, salmon, swordfish, trout, sardines
- Histamine is not broken down by cooking, freezing
- Storing fish at 20°C for 2-3 hours is enough to result in poisoning
- Bacteria reposnsible: E. coli, K. pneumoniae, halophilic Vibrio sp., Proteus, Clostridium and Salmonella, and Shigella
- Fish appear to have honey-combed scales and taste “peppery”, “bubbly” or “spicy”
- Raw milk contaminated before production of Swiss sheese results in siilar bacterial overgrowth and histamine build-up
Scombroid rash
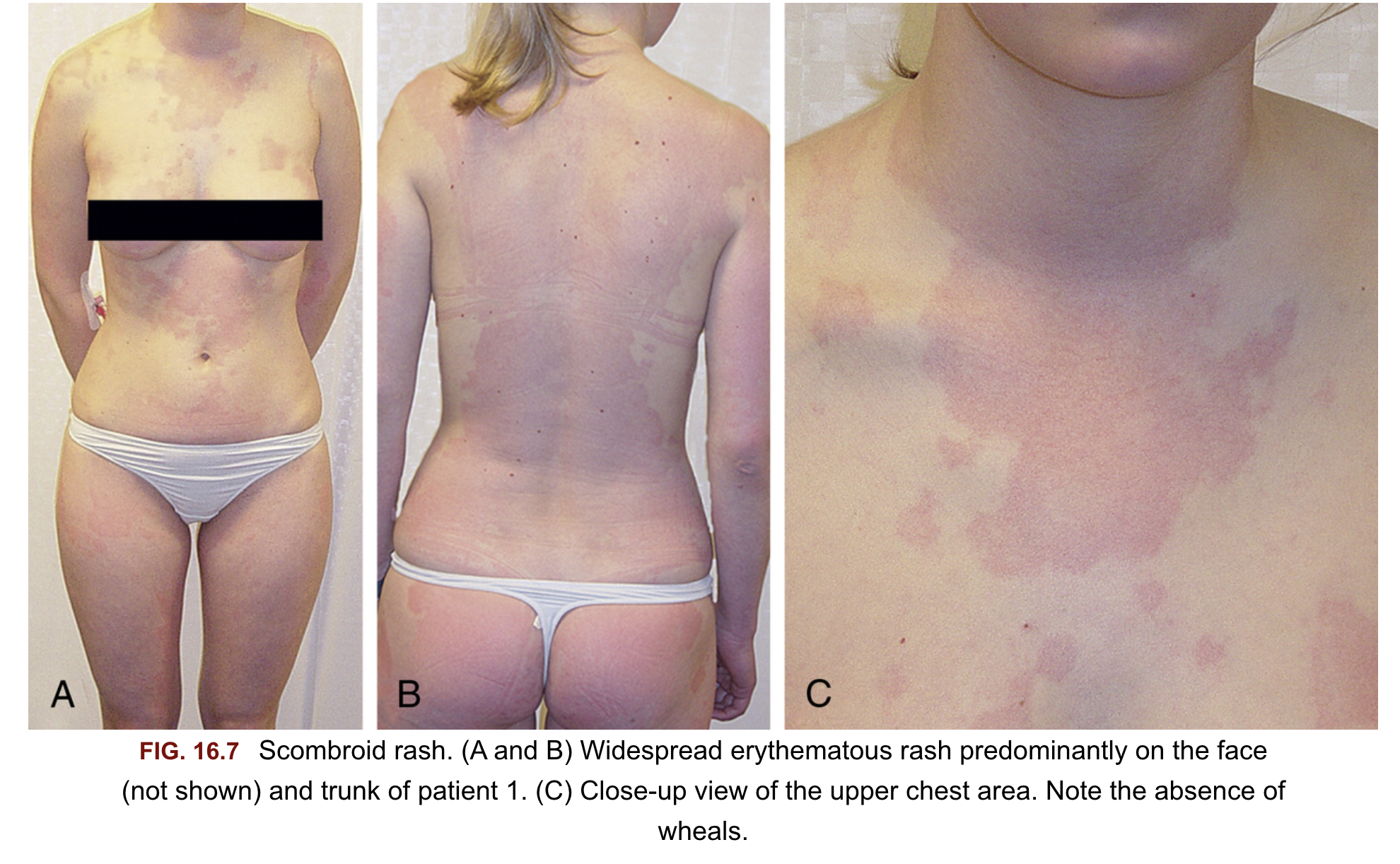
Spec et al. Comprehensive review of infectious diseases
Ciguatera
- Foodborne illness caused by consumption of reef fish (barracuda, amberjack, moray eel, some types of grouper, snapper, parrotfish) contaminated with multiple toxins, including ciguatera toxin, which arises from dinoflagellates
- Toxins accumulate in flash and organs
- Do not look, smell or taste different unlike scombroid poisoning
- Presents with GI symptoms and neurologic signs without altered mental status
Management summary
Evaluation of acute diarrhea in adults
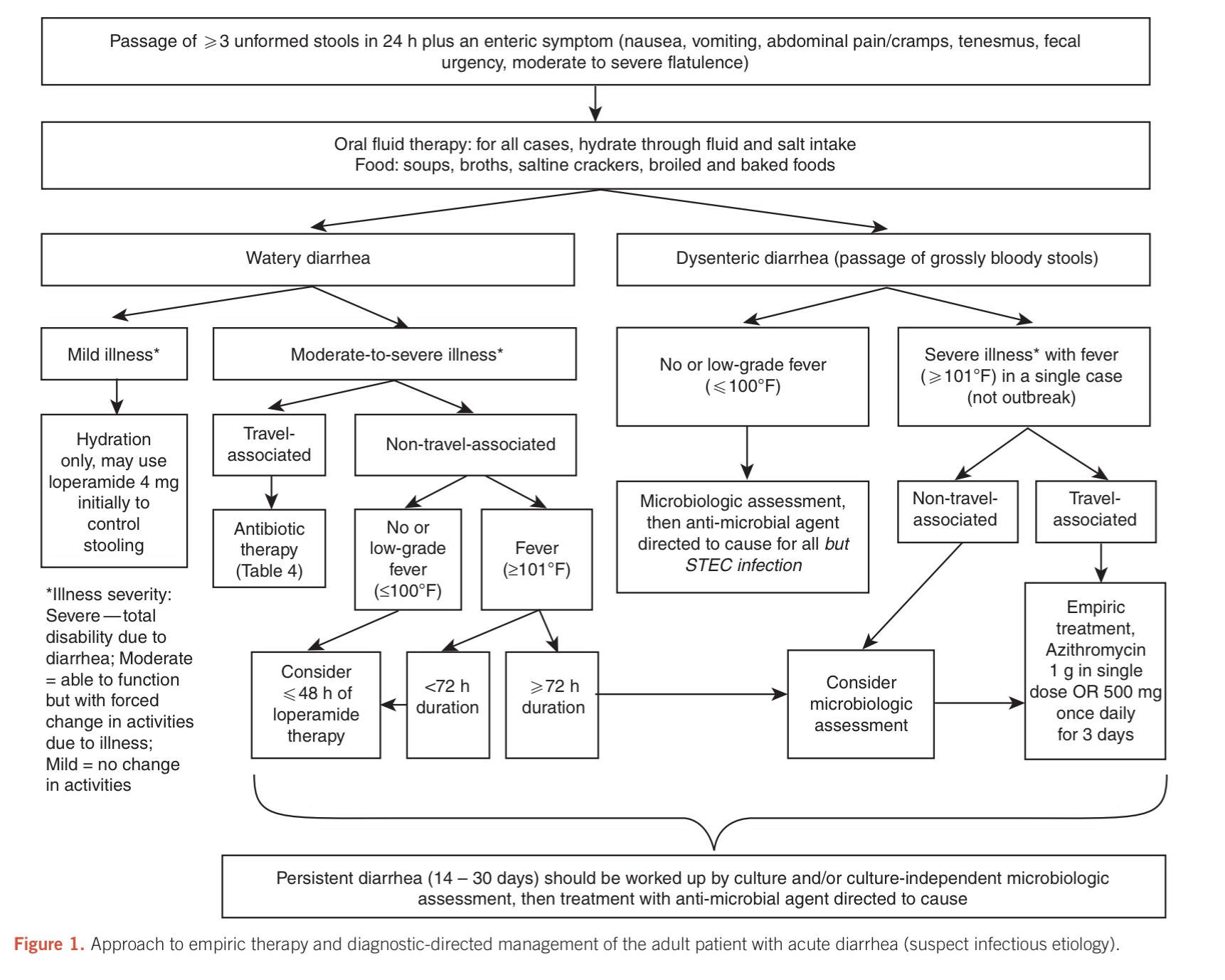
When should patient be evaluated in clinic?
Extraintestinal manifestations
- Symptoms:
- Persistent fever
- Bloody diarrhea
- Severe abdominal pain
- Symptoms of volume depletion (eg, dark or scant urine, symptoms of orthostasis)
- History of inflammatory bowel disease
- Hospitalization should be considered:
- History of immunosuppression (e.g., treatment for malignancy, transplantation, HIV
- Significant cardiovascular diseases
Causes of acute infectious diarrhea in adults in resource-rich settings
| Likely pathogens | Mean incubation period | Classic/ common food sources | Other epidemiologic clues | |
|---|---|---|---|---|
| Watery diarrhea | Norovirus | 24 to 48 hours | -Shellfish, prepared foods, vegetables, fruit | Outbreaks in: - Restaurants - Health care facilities - Schools and childcare centers - Cruise ships - Military populations |
| Clostridioides (formerly Clostridium difficile) | N/A | N/A | Antibiotic use - Hospitalization - Cancer chemotherapy - Gastric acid suppression - Inflammatory bowel disease |
|
| Clostridium perfringens | 8 to 16 hours | Meat, poultry, gravy, home-canned goods | ||
| Enterotoxigenic Escherichia coli (ETEC) | 1 to 3 days | Fecally contaminated food or water | -Travel to resource-limited settings | |
| Other enteric viruses (rotavirus, enteric adenovirus, astrovirus, sapovirus) | 10 to 72 hours | Fecally contaminated food or water | -Daycare centers -Gastroenteritis in children -Immunocompromised adults |
|
| Giardia lamblia | 7 to 14 days | Fecally contaminated food or water | -Daycare centers -Swimming pools -Travel, hiking, camping (particularly when there is contact with water in which beavers reside) |
|
| Cryptosporidium parvum | 2 to 28 days | Vegetables, fruit, unpasteurized milk | -Daycare centers -Swimming pools and recreational water sources - Animal exposure -Chronic diarrhea in advanced HIV infection |
|
| Listeria monocytogenes | 1 day (gastroenteritis) | Processed/delicatessen meats, hot dogs, soft cheese, pâtés, and fruit | -Pregnancy -Immunocompromising condition -Extremes of age |
|
| Cyclospora cayetanensis | 1 to 11 days | Imported berries, herbs | -Chronic diarrhea in advanced HIV infection | |
| Inflammatory diarrhea (fever, mucoid or bloody stools)¶ |
Nontyphoidal Salmonella | 1 to 3 days | -Poultry, eggs, and egg products, fresh produce, meat, fish, unpasteurized milk or juice, nut butters, spices | -Animal contact (petting zoos, reptiles, live poultry, other pets) -Travel to resource-limited settings |
| Campylobacter spp | 1 to 3 days | Poultry, meat, unpasteurized milk | -Travel to resource-limited settings -Animal contact (young puppies or kittens, occupational contact) |
|
| Shigella spp | 1 to 3 days | Raw vegetables | -Daycare centers Crowded living conditions -Men who have sex with men -Travel to resource-limited settings |
|
| Enterohemorrhagic E. coli (EHEC) | 1 to 8 days | Ground beef and other meat, fresh produce, unpasteurized milk and juice | -Daycare centers -Nursing homes -Extremes of age |
|
| Yersinia spp | 4 to 6 days | Pork or pork products, untreated water | -Abnormalities of iron-metabolism (eg, cirrhosis, hemochromatosis, thalassemia) -Blood transfusion |
|
| Vibrio parahemolyticus | 1 to 3 days | Raw seafood and shellfish | Cirrhosis | |
| Entamoeba histolytica | 1 to 3 weeks | Fecally contaminated food or water | Travel to resourcelimited settings Men who have sex with men |
Clostridioides (formerly Clostridium) difficile can also present with inflammatory diarrhea.
¶ Pathogens that are more classically associated with inflammatory diarrhea can also cause watery diarrhea, particularly early in the course of infection.
Patient Medical History
Patient Medical History
- Duration of symptoms
- Frequency and characteristics of stool
- Associated Symptoms
- Evidence of extracellular volume depletion (e.g., dark of scan urine, decreased skin turgor, orthostatic hypotension)
Small Bowel vs. Colon
- Diarrhea of small bowel is typically:
- Watery
- Large volume
- Accompanied by abdominal cramping, bloating and gas
- Diarrhea of large intestine is typically: - Frequent - Regular - Small volume - Painful - Bloody or mucoid stools (red blood and inflammatory cells seen in stool microscopy)
- Caveat: Patients can have both small and large bowel involvement
Small Bowel vs. Colon
| Pathogen | Small bowel | Colon |
|---|---|---|
| Bacteria | Salmonella Escherichia coli¶ Clostridium perfringens Staphylococcus aureus Aeromonas hydrophila Bacillus cereus Vibrio cholerae |
Campylobacter Shigella Clostridioides difficile Yersinia Vibrio parahaemolyticus Enteroinvasive E. coli Plesiomonas shigelloides Klebsiella oxytoca (rare) |
| Virus | Rotavirus Norovirus Astrovirus |
Cytomegalovirus* Adenovirus Herpes simplex virus |
| Protozoa | *Cryptosporidium Microsporidium _Cystoisospor*a_ Cyclospora Giardia lamblia |
Entamoeba histolytica |
¶ EPEC, EAggEC, EHEC, ETEC may all contribute; routine laboratories and cultures will not differentiate these from E. coli which are normal flora
Inflammatory signs: large-bowel infection
Fever, bloody or mucoid stools suggest invasive bacteria (eg, Salmonella, Shigella, or Campylobacter), enteric viruses (eg, cytomegalovirus [CMV] or adenovirus), Entamoeba histolytica, or C. difficile.
- Bloody stools, think: Shiga toxin-producing E. coli (STEC) (eg, E. coli O157:H7) infection.
- Other bacterial causes of visibly bloody diarrhea are Shigella, Campylobacter, and Salmonella species.
- Bloody diarrhea can also reflect noninfectious etiologies such as inflammatory bowel disease or ischemic colitis.
- Syndromes that begin with diarrhea but progress to fever and systemic complaints, such as headache and muscle aches, should raise the possibility of :
- Typhoidal illness (particularly in travellers from resource-limited settings)
- Listeria monocytogenes (particularly if a stiff neck is also present in pregnant patient)
Medical History: Exposures
- Food history
- Residence
- Occupational exposure
- Recent and remote travel
- Pets
- Hobbies
Food history
- Consumption of unpasteurized dairy products, raw or undercooked meat or fish, or organic vitamin preparations may suggest certain pathogens.
- The timing of symptom onset following exposure to the suspected offending food can be an important clue to the diagnosis
- Within six hours – suggests ingestion of a preformed toxin of Staphylococcus aureus or Bacillus cereus, particularly if nausea and vomiting were the initial symptoms
- At 8 to 16 hours – suggests infection with Clostridium perfringens
- More than 16 hours – suggests either viral or other bacterial infection (eg, contamination of food with enterotoxigenic or STEC or other pathogens)
Major foodborne microbes by the principal presenting gastrointestinal symptom
| Major presenting symptom | Likely microbes | Incubation period | Likely food sources |
|---|---|---|---|
| Vomiting | S. aureus | 1 to 6 hours | Prepared food, eg, salads, dairy, meat |
| B. cereus | 1 to 6 hours | Rice, meat | |
| Norwalk-like viruses | 24 to 48 hours | Shellfish, prepared foods, salads, sandwiches, fruit | |
| Watery diarrhea | C. perfringens | 8 to 16 hours | Meat, poultry, gravy |
| Enterotoxigenic E. coli | 1 to 3 days | Fecally contaminated food or water | |
| Enteric viruses | 10 to 72 hours | Fecally contaminated food or water | |
| C. parvum | 2 to 28 days | Vegetables, fruit, unpasteurized milk, water | |
| C. cayetanensis | 1 to 11 days | Imported berries, basil | |
| Inflammatory diarrhea | Campylobacter spp | 2 to 5 days | Poultry, unpasteurized milk, water |
| Nontyphoidal Salmonella | 1 to 3 days | Eggs, poultry, meat, unpasteurized milk or juice, fresh produce | |
| Shiga toxin-producing E. coli | 1 to 8 days | Ground beef, unpasteurized milk and juice, raw vegetables, water | |
| Shigella spp | 1 to 3 days | Fecal contamination of food and water | |
| V. parahemolyticus | 2 to 48 hours | Raw shellfish |
Incubation period and likely food sources are shown for each.
Modified from Centers for Disease Control and Prevention. Diagnosis and management of food borne illness, a primer for physicians. MMWR Recomm Rep April 16, 2004 / 53(RR04);1-33
Other exposures
- Exposure to animals (poultry, turtles, petting zoos) has been associated with Salmonella infection.
- Travel to a resource-limited setting increases the risk of bacterial diarrhea and also informs the risk of certain parasitic infections
- Occupation in daycare centres has been associated with:
- infections with Shigella, Cryptosporidium, and Giardia.
- Rotavirus is a potential consideration, but decreased with vaccination
Additional Medical history
- Recent antibiotic use (as a clue to the presence of C. difficile infection)
- Other medications (such as proton pump inhibitors, which can increase the risk of infectious diarrhea)
- Predisposing conditions:
- Immunocompromised host or the possibility of nosocomial infection
- Medical history informing the likelihood of various pathogens
- Pregnancy increases the risk of listeriosis following consumption of contaminated meat products or unpasteurized dairy products approximately 20-fold
- Cirrhosis has been associated with Vibrio infection
- Hemochromatosis has been associated with Yersinia infection
Physical exam-1
- Exam focus- volume status and identifying complications
- Volume depletion can be suggested by:
- dry mucous membranes
- diminished skin turgor
- postural or frank reductions in blood pressure
- altered sensorium
- Volume depletion can be suggested by:
- These signs can be mild or absent with early hypovolemia
Physical exam-2
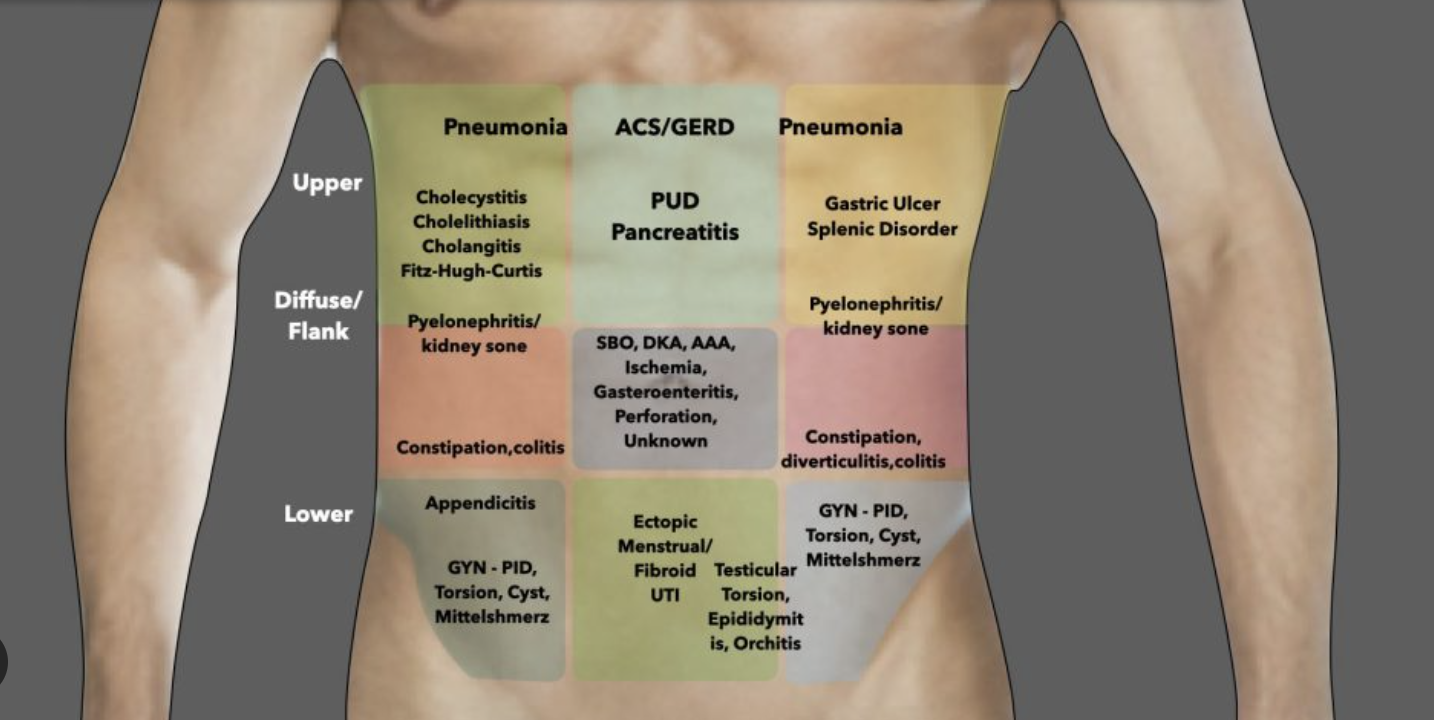
Abdominal examination should focus on signs that suggest ileus or peritonitis
- Abdominal distension
- Pain with gentle percussion
- Abdominal rigidity, or rebound tenderness
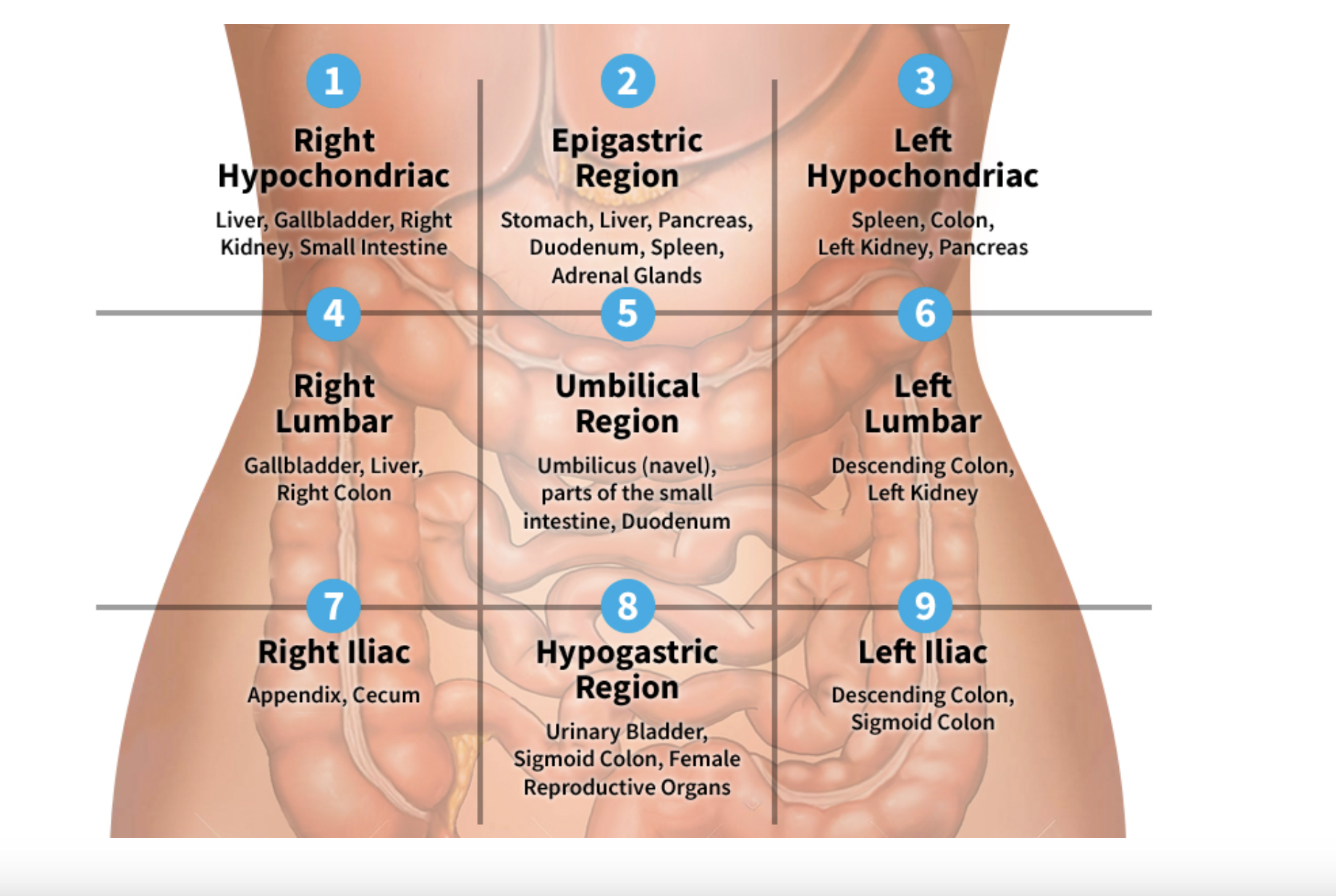
![]() {width=“600” center}
{width=“600” center}
Laboratory exam
- Laboratory tests are not routinely warranted for most patients with acute diarrhea
- If substantial volume depletion is present (suggested by signs or symptoms such as dark and concentrated urine), a basic metabolic panel should be performed to screen for hypokalemia or renal dysfunction
- The complete blood count does not reliably distinguish bacterial etiologies of diarrhea from others but may be helpful in suggesting severe disease or potential complications
- A low platelet count may prompt concern for the development of the hemolytic-uremic syndrome
- Leukemoid reaction is consistent with the diagnosis of C. difficile infection.
- Blood cultures should be obtained in patients with high fevers or who appear systemically ill
When are stool cultures considered?
- Severe illness
- Profuse watery diarrhea with signs of hypovolemia
- Passage of > 6 unformed stools per 24 hours
- Severe abdominal pain
- Need for hospitalization
- Other signs of symptoms concerning for inflammatory diarrhea
- Bloody diarrhea
- Passage of many small stools containing blood and mucus
- Temperature >38.5°
- High-risk host features
- Age ≥ 70 years
- Comorbidities such as cardiac disease (exacerbated by hypovolemia or complicating fluid replacement)
- Immunocompromised condition (including advanced HIV)
- Inflammatory bowel disease
- Pregnancy
- Symptoms persisting more than 1 week
- Suspected public health issue
Goal: Identify a potential bacterial pathogen that would inform the potential for complications and treatment decisions
Stool cultures
The optimal specimen for culture is a diarrheal stool specimen (conforms to container)o, which should be inoculated onto culture plates as quickly as possible.
Routine stool culture will identify Salmonella, Campylobacter, and Shigella
E. coli O157:H7 can be isolated on sorbitol-MacConkey plates or identified with antigen testing or polymerase chain reaction of stool
A stool culture that is positive for one of these pathogens in a patient with acute diarrheal symptoms can be interpreted as a true positive.
If a stool specimen cannot be obtained promptly, a rectal swab culture can be obtained to accelerate the diagnosis although some data suggest decreased sensitivity in adults
May need to specify bacteria of interest
- Campylobacter
- Aeromonas, Yersina
- Vibrio-requires selective media
Bacterial pathogens are generally excreted continuously, in contrast to ova and parasites, which are often shed intermittently.
Thus, a negative culture is usually not a false negative, and repeat specimens are rarely required.
Stool testing: molecular methods
- Multipathogen molecular panels — Some laboratories have access to multiplex stool tests, with which molecular tests for a panel of many different pathogens (bacterial, viral, and parasitic) can be performed simultaneously on diarrheal stool samples and, in some cases, rectal swab
Treatment
- Antibiotic specific recommendations per pathogen.
- Fluroquinolones, azithromycin, ceftriaxones (amoxicillin), trimethoprim-sulfamethoxazole, doxycycline
- Oral rehydration when possible vs. IV
Fluid repletion
- The most critical therapy in diarrheal illness is rehydration, preferably by the oral route, with solutions that contain water, salt, and sugar
- Diluted fruit juices and flavored soft drinks along with saltine crackers and broths or soups may meet the fluid and salt needs in patients with mild illness
- The electrolyte concentrations of fluids used for sweat replacement (eg, Gatorade) are not equivalent to oral rehydration solutions, although they may be sufficient for the otherwise healthy patient with diarrhea who is not hypovolemic.
- Oral rehydration solutions (ORS), including standard World Health Organization ORS or commercial ORS, such as Rehydralyte and Ceralyte, may be more appropriate in patients with more severe diarrheal disease. They should be used both to replete a volume depleted patient and also to maintain adequate volume status once replete.
Composition of oral rehydration solutions (ORSC) and commonly used beverages
| Carbohydrate (g/L) |
mEq/L | Osmolarity (mOSM/kg H2O) |
|||
|---|---|---|---|---|---|
| Sodium | Potassium | Base (HCO3–) | |||
| Oral rehydration solutions | |||||
| CeraLyte | 40 | 70 | 20 | 10 | 235 |
| Enfalyte | 30 | 50 | 25 | 30 | 200 |
| Pedialyte | 25 | 45 | 20 | 30 | 250 |
| Rehydralyte | 25 | 75 | 20 | 30 | 310 |
| WHO (1975) | 20 | 90 | 30 | 30 | 310 |
| WHO (2002) | 13.5 | 75 | 20 | 30 | 245 |
| Commonly Used Beverages (not appropriate for repletion therapy) | |||||
| Apple juice | 100 to 150 | 3 | 20 | 0 | 700 |
| Chicken broth | 0 | 250 | 5 | 0 | 450 |
| Colas | 100 to 150 | 2 | 0.1 | 13 | 550 |
| Gatorade | 45 | 20 | 3 | 3 | 330 |
| Ginger Ale | 90 | 3.5 | 0.1 | 3.6 | 565 |
| Tea | 0 | 0 | 0 | 0 | 5 |
ORSs were developed following the realization that, in many small bowel diarrheal illnesses, intestinal glucose absorption via sodium-glucose cotransport remains intact. Thus, in diarrheal disease caused by any organism that depends on small bowel secretory processes, the intestine remains able to absorb water if glucose and salt are also present to assist in the transport of water from the intestinal lumen
 {width=“600” center}
{width=“600” center}